Imagine booking your appointment, dreaming of a smile makeover, and then leaving the dentist’s chair with a hard no: “Sorry, dental implants aren’t suitable for you.” Most people assume dental implants are the golden ticket for missing teeth, but not everyone can—or should—get them. Here’s the real story behind why some people aren’t candidates and what you should know if you’re considering this life-changing step.
How Dental Implants Work—And Why They’re Not for Everyone
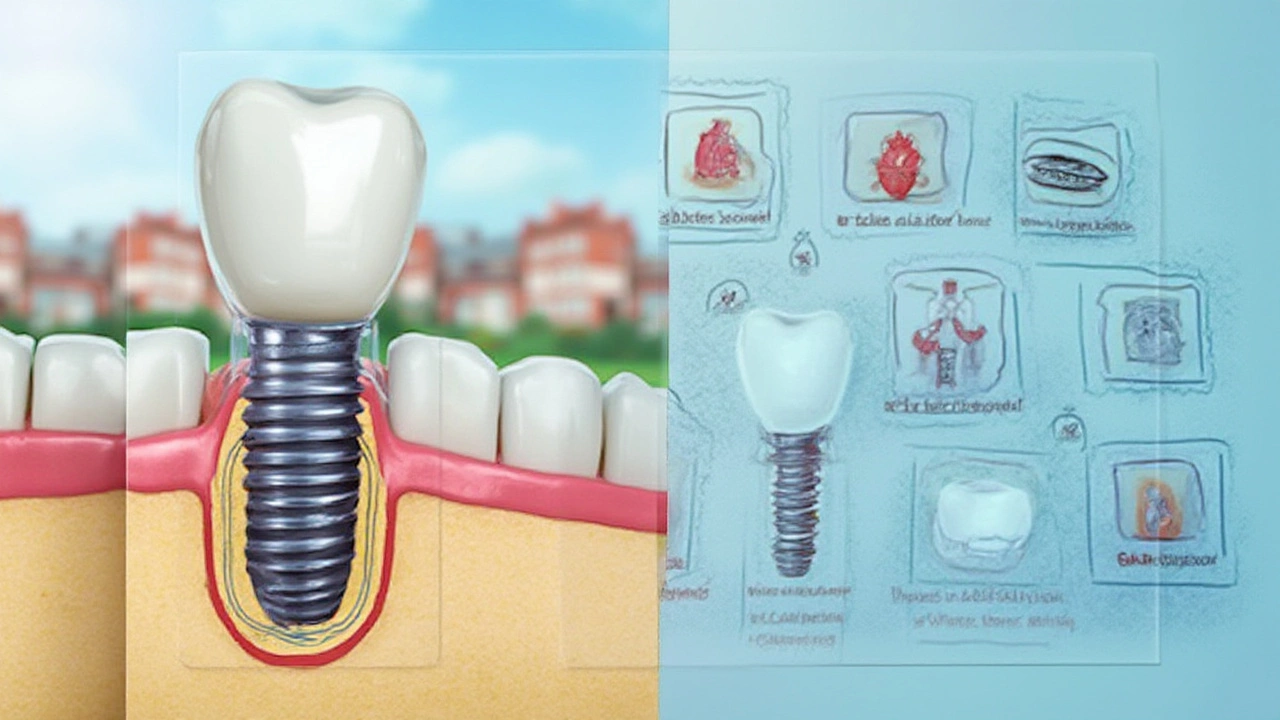
Dental implants sound almost futuristic—a titanium screw fuses to your jawbone and anchors a lifelike tooth that can last decades. Around 500,000 people in the US get them every year, so they’re hardly rare. The reason they’re so popular? They look and function like natural teeth. But not every mouth rolls out the red carpet for an implant. You need enough healthy bone. You must have healthy gums. And your body must be up for a little bit of surgical healing.
Say your jawbone is thin from years of missing teeth or gum disease. That’s a problem. The implant needs enough support, or it’s like putting a flagpole in the sand—eventually it’ll topple. Periodontal disease, or gum infections, can also fast-track implant failure. There’s no sense putting a pristine implant into a septic neighborhood.
Getting an implant means small, controlled surgery. Anyone with serious underlying health conditions (think uncontrolled diabetes or blood disorders) is automatically facing more risk. You don’t want an implant site that doesn’t heal or picks up an infection because your immune system’s not fighting back.
Let’s talk medications. Are you taking bisphosphonates for osteoporosis? Or heavy duty immune suppressants for autoimmune conditions? Both have been shown in studies to delay healing or increase the risk of implant failure, because they change how your body builds (and breaks down) bone. If you’re on regular steroids, blood thinners, or chemotherapy, your dentist will push pause before signing you up for surgery.
And finally, if you smoke, your risk of implant failure doubles. Studies since 2019 keep making it painfully obvious: nicotine plus surgery equals bad news for healing. If you plan to get an implant, quitting smoking is the single biggest thing you can do to tilt the odds in your favor.
Who Is Not a Good Candidate? Medical Issues and Lifestyle Factors
So, who lands in the “not a candidate” group?
- Uncontrolled health conditions: If your diabetes is out of control, your tissues just won’t heal at the normal pace. Same goes for blood disorders or immune system diseases that slow wound healing.
- Extensive bone loss: Not enough jawbone? No anchor for the implant. Sometimes bone grafts can fix this, but if the loss is too severe, even those may not work.
- Active gum disease: You can’t plant a seed in contaminated soil and expect a healthy flower. Gum infections make it far more likely you’ll lose the implant.
- Smoking and nicotine use: Science shows smokers have nearly twice the failure rate of non-smokers. Even vaping can slow healing.
- Alcohol and substance abuse: Healing gets harder and infection risk climbs with drug or heavy alcohol use.
- Recent heart attacks or strokes: Surgeons will usually wait 6–12 months after a major cardiac event before considering implants.
- Radiation to the jaw: If you’ve had cancer treatment with radiation in the mouth or jaw, your bone’s ability to heal can be permanently reduced.
- Pregnancy: Most dentists would rather wait until after baby arrives for elective surgery like dental implants.
Kids and teens aren’t good candidates either—their jawbones are still growing, so an implant can easily end up in the wrong place once their bones mature.
On the flip side, age alone isn’t a barrier. There are people in their 80s who heal beautifully, as long as their health and oral hygiene are on point. What matters more than the number of candles on your cake is what your medical history says about your body’s ability to heal and fight infection.
Medications do matter. For example, if you’ve taken bisphosphonates like Fosamax for osteoporosis—even for a few years—your risk of something called osteonecrosis (bone death) at the implant site goes up. That’s rare, but it’s one reason your dental team always asks about your meds. Same thing with SSRIs for depression: studies link these popular drugs to higher implant failure rates (possibly due to effects on bone metabolism), but doctors might weigh your mental health benefits against the small additional risk.
So, are all these risk factors going to automatically block you from ever getting an implant? Not always. But they do mean you need a much more tailored treatment plan, and sometimes the answer really is “no”—not this time, not this way.

What Tests Do Dentists Use to Decide If You’re a Candidate?
Newsflash: Dentists don’t just eyeball your jaw and say yes or no. They use a checklist and diagnostic tests to measure things like bone density, gum health, and your body’s ability to heal. You’ll usually start with a digital x-ray or, often, a 3D cone-beam CT scan. Why? Because these images show exactly how much jawbone you have, any hidden infection, and whether there’s room for an implant without hitting a nerve or sinus.
Next, dentists check your gums with a probe for pocket depth (think of this as how much space bacteria have to hide in). If it’s over 5mm, that’s a red flag for possible gum disease. They’ll also do a general oral hygiene check—are you the type to brush morning and night or more of a “whoops, forgot again” kind of brusher?
Medical history matters a lot. You might have to share more with your dentist than with your GP, including all medications and supplements. A lot of people overlook supplements like St. John’s Wort or ginseng, which can actually affect healing or interact with anesthesia.
Blood tests are rare unless something looks off, but if you have diabetes or other relevant conditions, your dentist might want to see your latest A1c result (for glucose control) or a clotting profile.
Sometimes, dentists will refer you for bone density tests, especially if you’re post-menopausal or have a history of osteoporosis. These tests aren’t just for hips—they can clue the team in if your jaw can handle surgery. In some cases, your doctor and dentist may actually chat about how your medications and overall health affect your dental plans.
If you ace all these, chances are high that an implant is worth the investment. But if something’s not right, your dentist will point it out—maybe you need gum surgery first, or to go see an endocrinologist, or to talk with your GP about medication changes. The idea isn’t to deny you a new smile, but to make sure you’re not set up for disappointment (and pain, and big dental bills).
What Are the Alternatives if Dental Implants Aren’t For You?
If the answer is still “implants aren’t safe for you,” don’t lose hope. Dentistry has thousands of ways to close a gap! The most familiar option is a bridge—an artificial tooth or teeth that anchors to your natural teeth on either side. Bridges can last 10 to 15 years and don’t need jawbone support—but they do require shaving down healthy teeth, which not everyone loves.
Removable partial dentures are another option. They attach to your remaining teeth with clasps. You take them out at night and soak them. Are they as comfortable or life-like as implants? Not usually, but today’s dentures look miles better than the wobbly plates your grandparents wore. Flexible resin partial dentures blend in better and don’t need metal wires.
Full dentures—the old “false teeth” stand-in—still work if you’re missing all your teeth. They cost less than implants and give back chewing power and speech, but can feel odd and need adjusting as your gums change over time.
Some people go for mini-implants, which use smaller screws and work for those with thin jawbones, though they’re not as strong as traditional implants. But if your jaw can’t handle any surgery, stick with non-invasive options.
You can even mix and match: some people wear partial dentures until bone grafts heal enough for an implant down the road. Don’t forget about orthodontics, too—moving teeth to close gaps works in some cases, especially if you still have a full set of healthy molars and front teeth.
One unexpected perk: often, being told you’re not a candidate for implants shines a spotlight on other untreated health problems, like undiagnosed diabetes or long-standing gum disease. Fixing those puts you in a better place generally—sometimes making it possible to revisit dental implants later.
How to Improve Your Chances of Successful Dental Implants
You want to tip the odds in your favor? Instead of treating dental implants like a sudden fix, think long-term. Start by getting gum health in check. Daily flossing and using a mouthwash with proven antibacterial action can clean out the crevices implants love to hide bacteria in. Electric toothbrushes, according to a large German study in 2023, remove up to 20% more plaque—so investing in a good one pays off.
Quit smoking now. Don’t just cut back—quit for at least two months before surgery, and don’t start again during healing. It’s the “strongest single predictor” of implant failure, according to dental research published in the Journal of Clinical Periodontology, so don’t let one habit ruin your investment.
If you’re on tricky medications—like steroids, immune suppressants, or bisphosphonates—talk to your doctor and dentist as a duo. Sometimes switching meds, pausing certain drugs, or managing dosage can lower your risk and make surgery safer.
Mind your A1c if you have diabetes. Numbers under 7.0% make good healing far more likely, while anything over 8.0% raises the risk of post-op infections and failed implants. Your dental team might delay surgery until your numbers hit a safe range.
If your jawbone is too thin, ask about bone grafting. It’s a bit like gardening: adding rich “soil” (bone or synthetic material) to help support a future implant. Bone grafts can add months to your timeline, but give you the best shot at a lasting result.
Once the implant is in, the care never stops. Scrupulous oral hygiene keeps bacteria at bay. See your dentist for checkups twice a year (sometimes even more if you’re high risk). If you grind your teeth at night, consider a bite guard—unmanaged grinding puts extra stress on implants, pushing them to fail.
One last tip: ask about 3D guided placement, not old-fashioned freehand surgery. Using a digital guide to place the implant improves accuracy, reduces complications, and can speed up healing, according to data from the Academy of Osseointegration 2024 summit. It’s more affordable than you might expect, especially since it spares you expensive corrections later.
So, who shouldn’t get dental implants? If you recognize any of the risk factors or fit into the "no-go" group, talk openly with your dentist. And if you're on the fence, prep your health as best you can—sometimes the "impossible" becomes possible when you get all the right info and tools. The finish line? A strong, lasting smile that’s really yours, for years to come.




