Supportive Check-in Tool
Assess your current approach to supporting someone struggling mentally with evidence-based techniques from the article.
How are you supporting them?
Your approach aligns with evidence-based support
You're doing exactly what research shows helps: listening without fixing, asking specific questions, or offering concrete help. This creates safety and encourages seeking professional support.
Why this works:
Studies show people who feel heard are 40% more likely to seek help. Your approach validates their experience without shifting focus to you.
Your approach could be improved
The article recommends avoiding vague questions like "Are you okay?" and comparison. These often lead to false reassurances that prevent real connection.
How to improve:
- Replace "Are you okay?" with specific questions like "What's been hardest this week?" to encourage truth
- Offer concrete help rather than open-ended invitations
- Use phrases like "I can't know what this feels like, but I want to understand"
Immediate action needed
Avoid comparing their pain to your experience or asking vague questions. These can make them feel dismissed or like a burden.
Critical adjustments:
When you notice signs of crisis (like feeling like a burden or discussing future plans), ask directly: "Are you thinking about hurting yourself?" This opens the door for help without judgment.
When someone you care about starts pulling away-skipping calls, canceling plans, staying silent at dinner-it’s easy to feel helpless. You want to fix it. But you can’t. And that’s okay. What you can do is show up. Not with solutions, not with advice, but with presence. Mental struggles don’t need fixing. They need witnessing.
Listen Without Trying to Fix It
Most people don’t need you to solve their depression, anxiety, or burnout. They need you to sit with them while they feel it. When someone says, “I just can’t get out of bed,” don’t respond with, “Have you tried exercise?” or “What if you just got up earlier?” That’s not support. That’s dismissal.Instead, say: “That sounds really heavy. I’m here.”
Studies show that people who feel heard during emotional crises are 40% more likely to seek professional help later. You don’t need to be a therapist. You just need to stop talking long enough to let them talk. Silence isn’t awkward-it’s safe.
Ask Specific Questions, Not Vague Ones
“Are you okay?” is a question people learn to answer with “Yeah, fine.” It’s a social default. It doesn’t invite truth.Try this instead:
- “What’s been the hardest part this week?”
- “Do you feel like you’ve had any moments of peace lately?”
- “Is there one thing that’s been weighing on you that you haven’t talked about?”
These questions don’t demand a big answer. They give space for small ones. And small truths are often the ones that open the door to bigger ones.
Don’t Compare Their Pain to Yours
“I went through something similar,” is well-intentioned-but it shifts the focus back to you. Mental health isn’t a competition. Someone’s panic attack isn’t less real because you once felt sad after a breakup.Instead of sharing your story, say: “I can’t know exactly what that feels like, but I want to understand.”
This simple phrase validates their experience without erasing it. It says: Your pain belongs to you. I’m not here to claim it.
Offer Concrete Help, Not Just “Let Me Know If You Need Anything”
When someone is drowning in low energy or brain fog, asking them to reach out for help is like asking them to swim to shore while they’re already sinking.Instead of saying, “Let me know if you need anything,” say:
- “I’m picking up groceries tomorrow. Can I bring you something?”
- “I’ll walk the dog with you on Thursday at 5, no pressure to talk.”
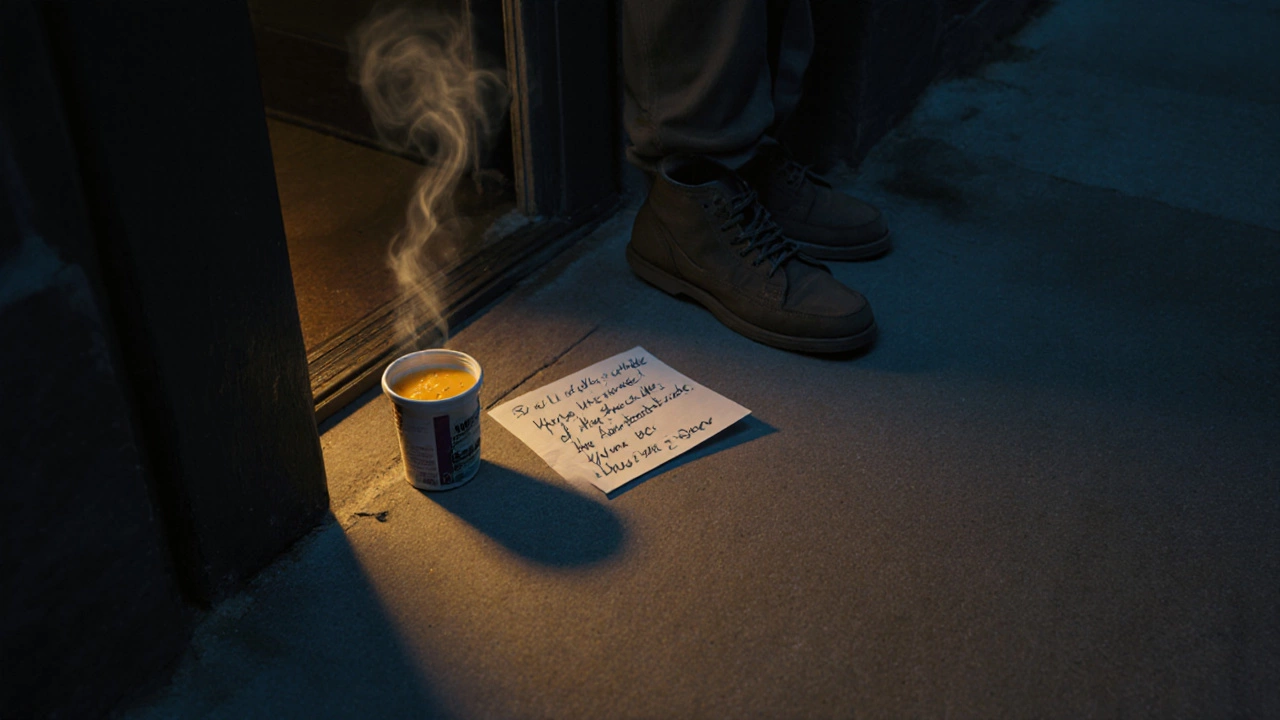
- “I made a soup. I’ll leave it on your porch tonight.”
These are actions, not invitations. They remove the burden of asking. And they show up in ways that matter-when the person can’t even text back.
Check In Regularly, Even If They Don’t Reply
One text a week can be the lifeline someone doesn’t know they’re holding onto. It doesn’t have to be long. Just: “Thinking of you. No need to reply.”People struggling with mental health often feel like a burden. They worry you’re tired of them. A consistent, low-pressure check-in tells them: “You’re not too much. I’m still here.”
It’s not about fixing their mood. It’s about reminding them they’re not alone in the dark.

Know the Warning Signs
Sometimes, support isn’t enough. If someone talks about:- Feeling like a burden to everyone
- Not seeing a future for themselves
- Planning how to end their life
-you need to act. Not gently. Not politely. Directly.
Ask: “Are you thinking about killing yourself?”
Yes, that’s hard to say. But it’s easier than losing someone. And asking doesn’t plant the idea. It opens the door. Most people who are suicidal feel relieved someone finally asked.
If they say yes, don’t leave them alone. Call a crisis line. Stay with them. Drive them to the ER. You don’t need to be an expert. You just need to be brave enough to care enough.
Take Care of Yourself Too
You can’t pour from an empty cup. Supporting someone mentally unwell is emotionally taxing. You’ll feel sad, frustrated, even angry. That’s normal.Set boundaries. Say no when you need to. Take breaks. Talk to someone else about how you’re feeling-just not about them. Protect your own mental space so you can keep showing up.
Supporting someone isn’t a marathon you run alone. It’s a team effort. You’re one player. You don’t have to carry it all.
It’s Not Your Job to Cure Them
You are not their therapist. You are not their medication. You are not their rescue.You are a person who cares. And that’s powerful enough.
Real change happens when someone feels safe enough to reach for help. Your role isn’t to fix them. It’s to make the world feel a little less scary so they can find their own way forward.
That’s enough. That’s everything.




