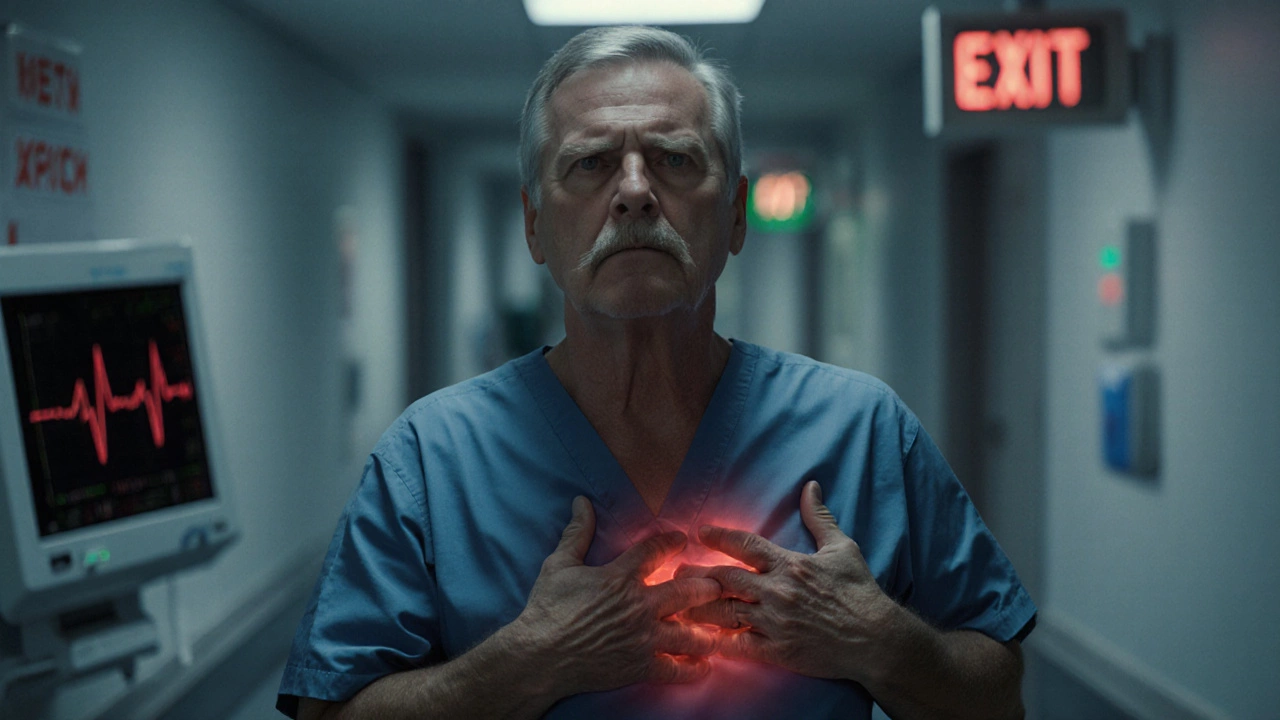
Emergency Pain Care: Quick Relief, Triage Tips & What to Expect
When you step into an Emergency Department with sudden, intense discomfort, Emergency Pain Care, the fast‑track service that aims to assess and ease severe pain within minutes. Also called acute pain management, it blends rapid evaluation, medication, and non‑pharmacologic tricks to keep you safe and comfortable.
Triage Protocols, the systematic steps nurses use to prioritize patients based on pain severity and overall risk are the backbone of any emergency setting. By quickly sorting who needs immediate intervention, these protocols cut waiting time and improve outcomes. When a nurse spots a high pain score, the next move is often a focused pain assessment.
Pain Assessment Tools, standardized scales like the Numeric Rating Scale or Visual Analogue Scale that translate a person's feeling into a number let clinicians gauge intensity, track changes, and decide on medication dosage. The data from these tools feeds directly into the triage decision, creating a clear link: Emergency Pain Care requires accurate assessment, which in turn drives appropriate medication.
Once the pain level is charted, Pain Medication, opioids, NSAIDs, or regional blocks prescribed in the ER becomes the first line of defense. Studies show that timely analgesics reduce the risk of chronic pain development. But medication isn’t the only answer; many hospitals pair it with Non‑Pharmacologic Relief, methods like cold packs, positioning, or breathing techniques to enhance comfort and lower drug doses.
All these pieces—triage, assessment, medication, and supportive measures—form a tight loop: Emergency Pain Care encompasses rapid assessment, which triggers targeted medication, which is amplified by non‑drug strategies. Understanding this flow helps you know what to expect the moment you arrive at the ER. Below you’ll find articles that break down each step, compare medication options, share real‑world triage stories, and offer home‑ready tips for managing pain after you leave the department.