Pain Relief Strategy Selector
Your Recommended Pain Relief Plan
Action Steps
When unbearable pain hits, it feels like your whole world narrows down to that single, crushing sensation. You might wonder whether you should wait for a doctor, call an ambulance, or try a home remedy first. This guide walks you through short‑term fixes you can apply right now, plus the steps to build a lasting plan that keeps the pain from stealing your life.
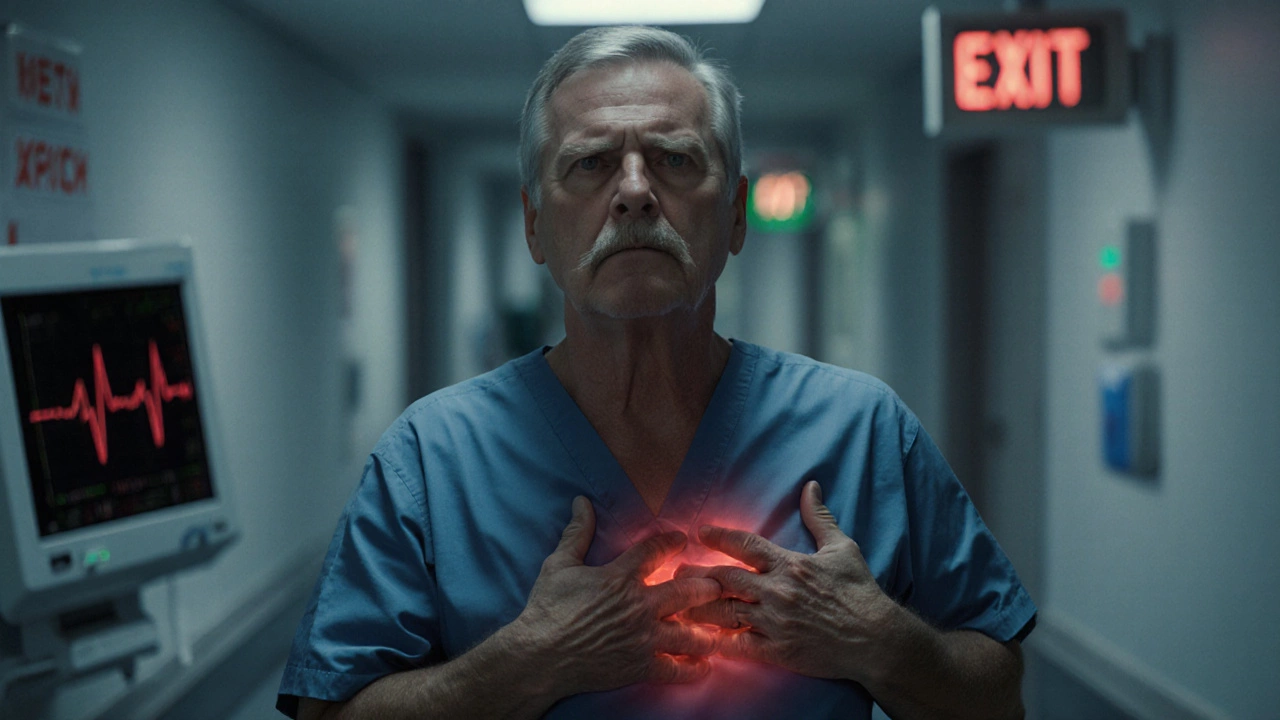
Recognise When Pain Is an Emergency
First, let’s separate a true emergency from a severe but non‑life‑threatening episode. Unbearable pain is an intense, often sudden sensation that overwhelms normal coping mechanisms and may signal a serious underlying condition can be a red flag for heart attack, stroke, internal bleeding, or a severe infection. If the pain appears with symptoms like chest tightness, shortness of breath, sudden weakness, loss of consciousness, or a high fever, dial emergency services immediately.
Quick‑Fix Tactics for Immediate Relief
When the pain isn’t a medical emergency, you still need fast action. Below are five practical steps you can try within minutes:
- Cold or heat application: Ice reduces inflammation for acute injuries, while a warm compress eases muscle spasm.
- Controlled breathing: Inhale for four counts, hold for two, exhale for six. This simple rhythm can lower the pain signal intensity in the brain.
- Gentle movement: Even a short walk or light stretching can release endorphins and prevent the pain from locking you into a static, painful posture.
- Over‑the‑counter (OTC) analgesics: Ibuprofen, naproxen, or acetaminophen can blunt pain pathways temporarily. Follow dosing instructions carefully.
- Distraction techniques: Engaging with a favorite song, a short video, or a simple puzzle diverts attention away from pain signals.
These measures are not cures, but they can bring the intensity down enough for you to think clearly about the next steps.
Medication Options: Safety First
If OTC drugs aren’t enough, you might consider prescription medication. Opioids are strong pain relievers that bind to brain receptors, reducing the perception of pain but carrying risks of dependence and side effects are reserved for severe cases and usually for short durations. Discuss dosage, potential interactions, and tapering plans with your prescriber.
Other prescription categories include:
- Antidepressants (e.g., duloxetine) - useful for neuropathic pain.
- Anticonvulsants (e.g., gabapentin) - also target nerve‑related pain.
- Topical agents (e.g., lidocaine patches) - provide localized numbness without systemic effects.
Always keep a medication list handy and review it with a pharmacist to avoid dangerous combos.

Physical Therapies That Move Pain Out of the Way
For many, the body’s own mechanics are the secret weapon against relentless pain. Physical therapy involves guided exercises, manual techniques, and education to restore movement, strength, and function can transform a painful day into a productive one. A qualified therapist will assess your posture, gait, and muscle imbalances, then prescribe a program that usually includes:
- Stretching tight muscles that pull on joints.
- Strengthening surrounding muscles to offload stressed structures.
- Manual mobilisations that improve joint range of motion.
- Education on ergonomic adjustments for work and home.
Even a few sessions can reduce reliance on medication and empower you with self‑care tools.
Mind‑Body Approaches: Training the Brain to Calm Pain
Pain isn’t just a physical signal; it’s processed in the brain, where emotions and thoughts can amplify or soothe it. Two evidence‑based techniques stand out:
Cognitive Behavioral Therapy teaches patients to identify and reframe negative pain‑related thoughts, reducing emotional distress and perceived pain intensity helps break the cycle of catastrophizing. A typical CBT session includes:
- Discovering thought patterns that worsen pain.
- Learning coping statements such as “I can tolerate this discomfort for a few minutes.”
- Developing activity pacing to avoid boom‑bust cycles.
Another accessible tool is Mindfulness practice that cultivates non‑judgmental awareness of the present moment, helping the brain distance itself from the pain narrative. Simple daily habits-like a 10‑minute guided body scan or mindful breathing-have been shown to lower pain scores by up to 30% in chronic sufferers.
Building a Long‑Term Pain Management Plan
Short‑term relief is only half the battle. For lasting control, assemble a multidisciplinary team centered around a Pain management specialist is a clinician-often an anesthesiologist, neurologist, or physiatrist-trained to evaluate complex pain and coordinate comprehensive treatment. Here’s how to structure the plan:
- Comprehensive assessment: Identify whether the pain is acute (lasting less than six weeks) or chronic (persisting longer). Acute pain typically signals tissue injury and usually resolves with proper healing may need different strategies than Chronic pain is a persistent condition that often involves central sensitisation and requires multimodal therapy.
- Tailored medication regimen: Combine low‑dose opioids (if absolutely necessary) with adjuvant drugs, monitoring for side effects.
- Physical and occupational therapy: Set functional goals, such as walking 500 meters without flare‑ups.
- Psychological support: Incorporate CBT or acceptance‑commitment therapy to reduce fear‑avoidance behaviours.
- Lifestyle optimisation: Address sleep hygiene, nutrition (anti‑inflammatory foods like oily fish), and stress management.
Regular follow‑ups-every 4-6 weeks initially-allow the team to tweak each component based on your progress.

Practical Lifestyle Tweaks That Make a Difference
Small daily habits often have outsized impact on pain perception:
- Sleep routine: Aim for 7-9 hours in a dark, cool room. Consider a cervical pillow if neck pain is a trigger.
- Anti‑inflammatory diet: Include turmeric, ginger, berries, and leafy greens. Limit processed sugars and trans fats.
- Hydration: Dehydrated muscles are more prone to cramping and stiffness.
- Regular low‑impact cardio: Swimming, cycling, or brisk walking improves circulation and endorphin release.
- Posture checks: Set reminders to sit tall at work; use ergonomically designed chairs.
Tracking these habits in a simple journal can reveal patterns-like a flare‑up after a night of poor sleep-helping you pre‑empt pain spikes.
Comparison: Immediate vs Long‑Term Relief Strategies
| Aspect | Immediate (Minutes‑Hours) | Long‑Term (Weeks‑Months) |
|---|---|---|
| Goal | Reduce intensity enough to function | Prevent recurrence and improve quality of life |
| Typical tools | Cold/heat, breathing, OTC meds, distraction | Physical therapy, CBT, medication optimisation, lifestyle changes |
| Professional input | Pharmacist or urgent‑care nurse (if needed) | Pain specialist, physiotherapist, psychologist, dietitian |
| Risk level | Low (unless misuse of meds) | Variable - depends on medication side effects and therapy adherence |
| Monitoring | Self‑assessment of pain score | Regular clinical reviews + symptom diary |
Next Steps for Different Scenarios
If you’re alone and the pain spikes suddenly: Try cold or heat, take an OTC analgesic, and call emergency services if you notice chest, abdominal, or neurological warning signs.
If you’re managing a known chronic condition: Schedule a review with your pain specialist, update your medication list, and add one new mind‑body practice (e.g., 10‑minute mindfulness) this week.
If you’ve tried everything and still feel stuck: Ask for a referral to a multidisciplinary pain clinic. These centers combine medical, physical, and psychological expertise under one roof, often delivering faster progress than fragmented care.
Frequently Asked Questions
Can I use opioids for unbearable pain without getting addicted?
Short‑term, low‑dose opioid courses can be safe when closely monitored by a doctor. The key is a clear taper plan and regular assessments for signs of dependence.
What’s the difference between acute and chronic pain?
Acute pain usually lasts under six weeks and signals tissue damage that’s healing. Chronic pain persists beyond that window, often involving changes in the nervous system that keep the sensation alive even after the original injury has healed.
Are over‑the‑counter drugs enough for severe pain?
OTC NSAIDs or acetaminophen can help many, but if pain stays high after the recommended dose, it’s a sign you should see a doctor for stronger or combination therapy.
How quickly can CBT reduce pain?
Most people notice a modest drop in pain intensity within 4-6 weeks of weekly CBT sessions, especially when they apply the coping skills daily.
Is mindfulness safe for everyone?
Yes, mindfulness is non‑invasive and generally safe. If you have active psychosis or severe depression, check with a mental‑health professional first.