Private Healthcare Cost Calculator
Calculate your potential out-of-pocket costs for private healthcare services. Enter your service fees and insurance coverage to see what you might pay out of pocket.
Your Estimated Costs
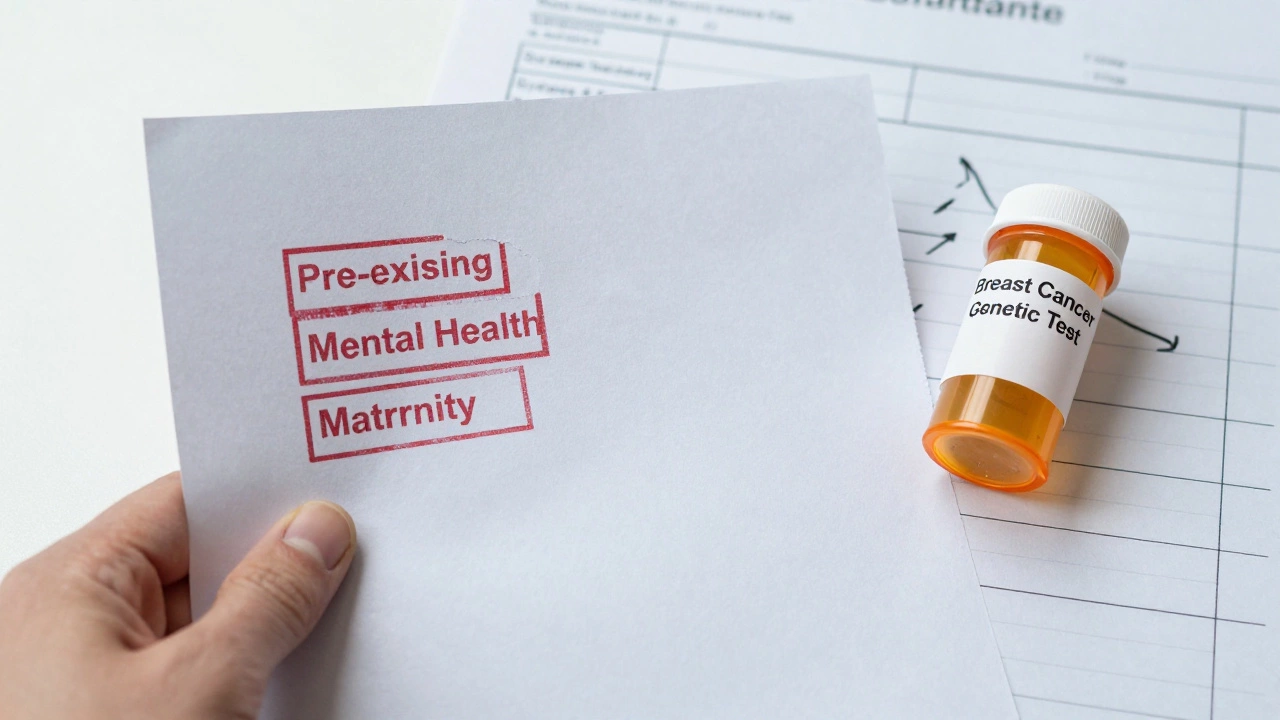
In 2024, 38% of private policyholders had claims denied. Common exclusions include mental health, maternity care, and pre-existing conditions.
Private healthcare sounds appealing at first glance. Faster appointments, private rooms, choice of doctors - it feels like a better deal. But beneath the surface, there are real downsides that many people don’t talk about until they’re stuck in the system. If you’re considering private healthcare, you need to know what you’re signing up for.
It’s expensive - and not just upfront
The biggest shock isn’t just the initial cost. It’s how the costs keep adding up. A private consultation might cost €150, but if you need an MRI, that’s another €500. A specialist referral? Another €300. And if something goes wrong - a complication, a misdiagnosis - you’re on your own for follow-up care. Insurance doesn’t always cover everything, and many policies have exclusions for pre-existing conditions, mental health, or maternity care. People often think they’re buying peace of mind, but they’re really buying a bill that keeps growing.
Access isn’t equal - it’s for those who can pay
Private healthcare doesn’t fix inequality; it deepens it. In Ireland, while the public system struggles with wait times, private patients jump ahead. This creates a two-tier system where your health outcomes depend more on your bank account than your medical need. A person with diabetes, for example, might get a private endocrinologist in days. Someone on the public system waits six months. That delay can mean nerve damage, amputation risk, or worse. The system isn’t designed to serve everyone - it’s designed to serve those who can afford it.
Insurance gaps leave people vulnerable
Most people assume private healthcare means insurance covers everything. It doesn’t. Policies often exclude chronic conditions, long-term rehabilitation, or even certain medications. A 2024 report from the Irish Health Insurance Authority found that 38% of private policyholders had at least one claim denied in the past year. Common reasons? Pre-existing conditions, experimental treatments, or services labeled “non-essential.” One woman in Cork paid €800 a month for coverage - then got diagnosed with early-stage breast cancer. Her policy wouldn’t cover the genetic testing her doctor recommended. She ended up going public for that part. That’s not a safety net. It’s a loophole.
Fragmented care can hurt your health
Private healthcare often means seeing different doctors in different clinics. No one central system tracks your full history. Your GP might not even know what specialist you saw. Test results don’t automatically transfer. Medications prescribed in one place might clash with ones from another. A 2025 study in the Irish Journal of Medical Science found that patients using private services had a 22% higher chance of medication errors simply because their records weren’t shared. In a public system, your records follow you. In private, you become your own coordinator - and most people aren’t trained to do that.
It can make you ignore the public system entirely
When you’re paying for private care, you start to believe the public system is broken. You stop advocating for improvements. You stop voting for better public funding. You stop complaining about long waits - because you’re not the one waiting. That’s dangerous. Private healthcare thrives when public healthcare weakens. The more people leave, the less political pressure there is to fix the public system. And when you need it - because you lose your job, get sick, or can’t afford premiums anymore - you’re suddenly on the other side. And it’s worse than ever.

Quality isn’t guaranteed - just faster
Just because you pay more doesn’t mean you get better care. A 2023 analysis of surgical outcomes across private clinics in Dublin showed no significant difference in success rates compared to public hospitals for common procedures like knee replacements or gallbladder removals. The only difference? Wait times. Private clinics often prioritize quick turnover. That means less time spent explaining options, less follow-up, and more pressure to discharge patients early. One patient in Limerick had a private hip surgery, was sent home after 24 hours, and developed a serious infection because no one checked in. Public hospitals had protocols for monitoring. Private ones didn’t.
It doesn’t scale - and it’s unsustainable
Private healthcare works for individuals, but not for society. As more people leave the public system, it gets less funding, fewer staff, and longer waits. That pushes even more people toward private options - creating a spiral. In 2025, Ireland’s private healthcare sector grew by 14% - but public hospital funding only rose by 2%. That gap isn’t sustainable. It’s not just unfair. It’s a ticking time bomb.
What you’re really buying
Private healthcare isn’t about better medicine. It’s about speed, comfort, and control. But those things come at a steep price - financially, socially, and ethically. You’re not just paying for a doctor. You’re paying for a system that leaves others behind. And if your situation changes - if you lose your job, your insurance, or your health - you might find yourself in the very system you once dismissed.
Is private healthcare faster than public healthcare in Ireland?
Yes, for non-emergency care, private healthcare is usually faster. You can often see a specialist within days instead of months. But that speed doesn’t mean better outcomes. For many procedures, success rates are nearly identical between private and public hospitals. The difference is in access, not quality.
Can private health insurance deny claims?
Yes, and it happens more often than people think. In 2024, nearly 4 in 10 private policyholders in Ireland had at least one claim denied. Common reasons include pre-existing conditions, exclusions for mental health or maternity care, and treatments labeled "non-essential." Always read the fine print - coverage isn’t as broad as it seems.
Does private healthcare improve health outcomes?
Not necessarily. Studies show no major difference in recovery rates for common surgeries like hip replacements or appendectomies between private and public systems. The main advantage is quicker access, not better results. In fact, fragmented records in private care can lead to more medication errors and missed follow-ups, which can hurt long-term health.
Why does private healthcare make the public system worse?
When people leave the public system, they stop demanding better funding and staffing. That reduces political pressure to improve public services. As fewer people use public hospitals, funding drops, wait times grow longer, and morale among staff falls. This creates a cycle: the worse the public system gets, the more people flee to private care - making the public system even worse.
What happens if I lose my job and can’t afford private insurance?
You’ll be forced back into the public system - and it may feel like a step backward. You’ll face long wait times, limited specialist access, and possibly outdated facilities. Many people who left public care for private options find themselves overwhelmed when they return. The system doesn’t reset; it’s often worse than when you left.




