Chronic Pain Medication Comparison Tool
Understand Your Pain Treatment Options
This tool helps you compare common chronic pain medications based on your specific pain type, severity, and treatment history.
Select your pain profile to see recommended medications
Important Considerations
Combination Therapy
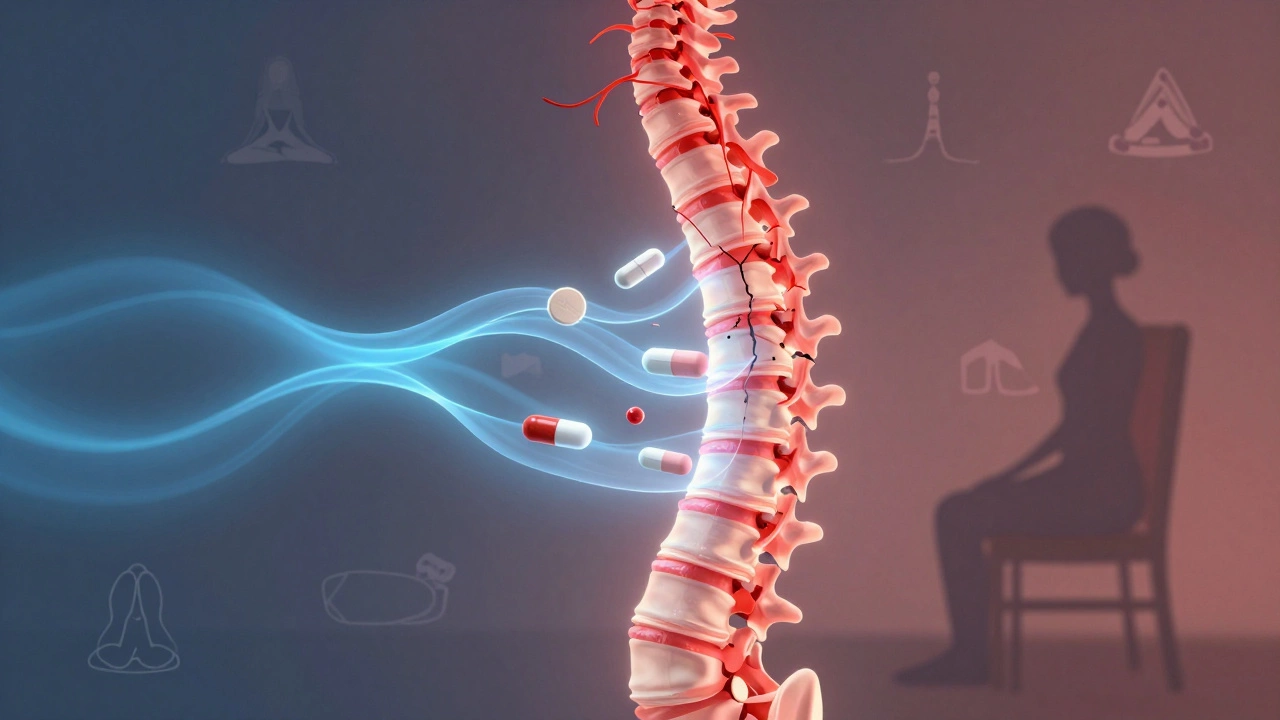
Most patients find success with combined treatments, not single medications. The article emphasizes that combining medication with physical therapy, psychological support, and lifestyle changes yields significantly better results (40-60% better pain control).
Opioid Warning
Opioids are generally avoided for chronic non-cancer pain due to risks of dependence, tolerance, and overdose. They're only considered when other treatments fail and benefits clearly outweigh risks.
Severe chronic pain doesn’t go away after an injury heals. It lingers for months or years-sometimes for life. People living with it aren’t just dealing with discomfort; they’re fighting sleepless nights, lost jobs, and the slow erosion of their sense of self. When over-the-counter painkillers fail, doctors turn to stronger options. But what’s actually prescribed? And what does that really mean for the person taking it?
Antidepressants and Anticonvulsants for Nerve Pain
Not all chronic pain comes from damaged muscles or joints. A lot of it comes from nerves firing wrong signals-like a faulty alarm system stuck on loud. This is called neuropathic pain. It’s common in conditions like diabetic neuropathy, post-shingles pain, and spinal cord injuries.
Doctors often start with antidepressants like amitriptyline or duloxetine. These aren’t prescribed because the patient is depressed. They work by changing how the brain and spinal cord process pain signals. Amitriptyline, a tricyclic antidepressant, has been used for decades for nerve pain. Studies show it reduces pain by 30-50% in about half of users. Duloxetine, an SNRI, is FDA-approved specifically for diabetic nerve pain and chronic low back pain.
Anticonvulsants like gabapentin and pregabalin are equally common. Originally designed for seizures, they calm overactive nerves. Pregabalin (Lyrica) works faster and has fewer side effects than gabapentin, but both can cause dizziness, weight gain, and brain fog. Many patients report feeling "drunk" on these drugs, especially when starting. Dosing is slow-doctors increase it gradually to avoid side effects.
Opioids: The Controversial Last Resort
Opioids like oxycodone, morphine, and tramadol are powerful. They bind to receptors in the brain and spinal cord, blocking pain signals. For some-like cancer patients or those recovering from major surgery-they’re life-changing.
But for chronic non-cancer pain? Guidelines from the CDC, NICE (UK), and Ireland’s Health Service Executive all say the same thing: avoid them if possible. Long-term use leads to tolerance-you need more to get the same effect. Dependence is common. Addiction is real. And overdose risk doesn’t disappear.
That’s why opioids are rarely first-line. When prescribed, it’s usually at the lowest effective dose for the shortest time. Extended-release forms are avoided unless absolutely necessary. Tramadol is sometimes used because it’s weaker and has some antidepressant properties, but it still carries addiction risk. In Ireland, prescriptions for strong opioids like oxycodone require special authorization under the Misuse of Drugs Regulations.
Topical Treatments: Local Relief Without Systemic Risk
Some people can’t tolerate pills. Others need targeted relief-say, for arthritis in one knee or back pain that doesn’t radiate. That’s where topical treatments shine.
Capsaicin cream, made from chili peppers, depletes substance P, a chemical that sends pain signals. Applied daily, it can reduce pain after a few weeks. It burns at first-some patients quit because of that initial sting.
Lidocaine patches (like Lidoderm) numb the skin locally. They’re great for post-herpetic neuralgia. You stick one on the painful area for up to 12 hours a day. No drowsiness. No stomach upset. Just quiet relief.
There’s also diclofenac gel, a non-steroidal anti-inflammatory (NSAID) you rub on. It works better than oral NSAIDs for localized joint pain because it delivers the drug right where it’s needed, with less risk to the stomach or kidneys.
NSAIDs and Acetaminophen: Limited but Still Used
People assume NSAIDs like ibuprofen or naproxen are the go-to for chronic pain. But for severe, long-term pain? They’re often not enough-and risky over time.
Long-term NSAID use increases the chance of stomach ulcers, kidney damage, and heart problems. That’s why doctors limit them to short bursts or low doses, even for arthritis. Acetaminophen (paracetamol) is safer for the stomach but doesn’t reduce inflammation. It’s weak for nerve pain and offers little relief in severe cases. Still, it’s often tried first because it’s cheap, widely available, and has a low risk profile if used correctly.
Combination Therapy: Why One Drug Isn’t Enough
Chronic pain isn’t one thing. It’s a mix of inflammation, nerve damage, muscle tension, and emotional stress. That’s why single drugs often fail. The best results come from stacking treatments.
A typical plan might include: gabapentin for nerve pain, a low-dose amitriptyline for sleep and mood, a lidocaine patch for localized flare-ups, and occasional tramadol for breakthrough pain. Physical therapy, cognitive behavioral therapy (CBT), and gentle movement like swimming or tai chi are almost always added.
Studies show patients who combine medication with non-drug therapies report 40-60% better pain control than those on pills alone. The goal isn’t to eliminate pain completely-it’s to make it manageable enough to live again.
The Hidden Cost: Side Effects and Quality of Life
Every medication has a price. Gabapentin can make you clumsy. Amitriptyline causes dry mouth and constipation. Opioids shut down breathing during sleep. Topical creams sting. Antidepressants can make you feel emotionally flat.
And then there’s the mental toll. Many patients feel guilty for taking opioids. Others are stigmatized as "drug seekers." Some stop taking meds because they’re ashamed. Others can’t afford them-especially newer drugs like pregabalin, which still carry high out-of-pocket costs in Ireland even with a medical card.
Doctors who treat chronic pain know this. The best ones don’t just write prescriptions. They listen. They adjust. They ask: "What do you want to do with your life?" Not "How bad is your pain on a scale of 1 to 10?"

What Doesn’t Work Anymore
Some treatments once thought effective are now abandoned. Muscle relaxants like cyclobenzaprine? Too sedating, no long-term benefit. Corticosteroid injections for back pain? Only useful for short-term flare-ups, not ongoing pain. Long-term benzodiazepines? Dangerous and ineffective for pain.
The medical community has learned. The old model-"more pills, more pain relief"-is outdated. Modern pain management is multidisciplinary. It’s about function, not just numbness.
When to Ask for a Specialist
If you’ve tried two or three medications without relief, or if side effects are worse than the pain, it’s time to see a pain specialist. These are doctors trained in pain medicine-often anesthesiologists or neurologists with extra certification.
They can offer things general practitioners can’t: nerve blocks, spinal cord stimulators, intrathecal drug pumps, or access to clinical trials. They also coordinate with physiotherapists, psychologists, and occupational therapists to build a full plan.
Waiting times for pain clinics in Ireland can be long-sometimes over a year. But if your pain is disabling, ask your GP to refer you as urgent. You have a right to proper care.
Final Thought: Pain Is Personal
There’s no universal answer to "What’s prescribed?" One person’s miracle drug is another’s nightmare. What works for a 55-year-old with spinal stenosis won’t help a 30-year-old with fibromyalgia.
The key is patience, persistence, and partnership with your doctor. Don’t settle for a prescription that leaves you worse off. Don’t be afraid to say: "This isn’t working." The goal isn’t to erase pain-it’s to reclaim your life from it.
Can chronic pain be cured with medication?
Medication rarely cures chronic pain. It manages it. The goal is to reduce pain enough so you can move, sleep, work, and enjoy life again. For most people, long-term relief comes from combining drugs with physical therapy, psychological support, and lifestyle changes-not just pills.
Are opioids safe for long-term chronic pain?
Opioids are not considered safe for long-term use in most cases of chronic non-cancer pain. They carry high risks of dependence, tolerance, overdose, and reduced quality of life over time. Major health organizations, including the CDC and NICE, recommend avoiding them unless other treatments fail and the benefits clearly outweigh the risks.
Why are antidepressants used for pain?
Antidepressants like amitriptyline and duloxetine affect brain chemicals (serotonin and norepinephrine) that help regulate pain signals. They don’t treat depression in this context-they change how the nervous system processes pain. Studies show they reduce nerve pain by 30-50% in many patients, even without depression.
What’s the best non-drug treatment for chronic pain?
There’s no single best, but movement and therapy are the most effective. Gentle aerobic exercise (like walking or swimming), strength training, and cognitive behavioral therapy (CBT) have the strongest evidence. CBT helps reframe how you think about pain, reducing fear and improving coping. Many patients report better outcomes from these than from medication alone.
Can I get pain medication without a prescription in Ireland?
No. Strong pain medications like opioids, gabapentin, pregabalin, and even high-dose NSAIDs require a prescription in Ireland. Over-the-counter options are limited to paracetamol, low-dose ibuprofen, and topical creams like diclofenac gel. Even then, pharmacists can refuse to sell if they suspect misuse.
How long does it take for pain meds to work?
It varies. Topical creams and NSAIDs may help within hours. Antidepressants and anticonvulsants take weeks-often 4 to 8 weeks-to show full effect. Patience is key. Stopping too soon means you’ll never know if it works. Always give a medication at least 6 weeks at the right dose before deciding it’s ineffective.




