Anesthesia Safety Calculator
Personalized Anesthesia Safety Assessment
This tool estimates your anesthesia risk based on factors discussed in the article. Remember: this is for informational purposes only and not medical advice.
There’s no fixed number-no magic cap like "five times max"-when it comes to how many times you can go under anesthesia. But that doesn’t mean it’s risk-free every time. The real question isn’t how many times you can do it. It’s whether each time is safe for you.
It’s Not About the Count, It’s About the Condition
People often worry they’ll "use up" their anesthesia allowance, like a coupon that expires after five uses. That’s a myth. Anesthesia doesn’t work like a battery that wears out. Your body doesn’t store a quota of safe anesthetics. Instead, each time you go under, your medical team looks at your current health, your past reactions, and what’s being done to you.
Two people can both have had three surgeries under general anesthesia. One might be a 28-year-old athlete with no medical issues. The other might be a 72-year-old with diabetes, high blood pressure, and a history of heart arrhythmia. The second person faces higher risks-even if they’ve had anesthesia before. The number of times isn’t the issue. The state of your body is.
What Makes Anesthesia Riskier Over Time?
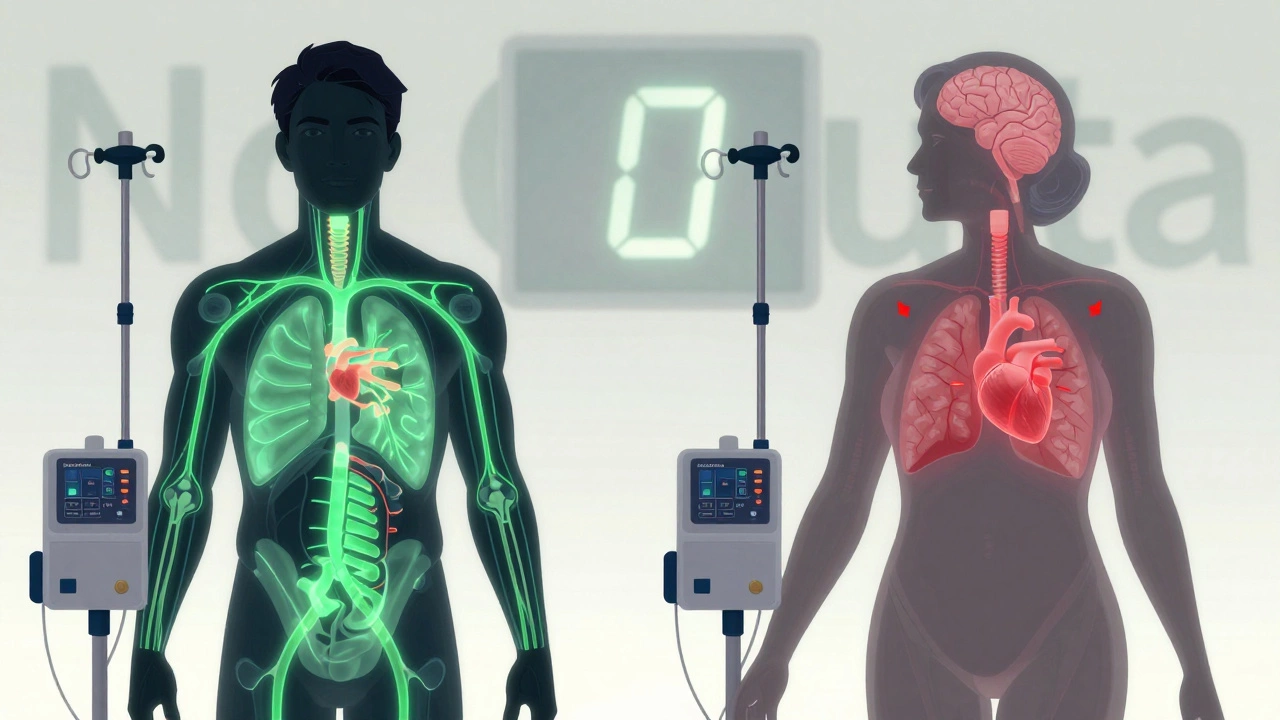
There are three big factors that raise the risk with repeated exposure: age, underlying health problems, and how your body responds to the drugs.
Aging changes how your body handles anesthesia. After 65, your liver and kidneys don’t clear drugs as quickly. Your brain becomes more sensitive to sedatives. Studies from the Mayo Clinic show older adults are more likely to experience postoperative delirium or cognitive decline after anesthesia-even after a single procedure. That risk grows with each exposure.
Chronic diseases matter more than repetition. If you have heart disease, COPD, obesity, or untreated sleep apnea, each anesthetic increases the chance of complications like low blood pressure, irregular heartbeat, or breathing problems. A 2023 study in Anesthesiology tracked over 120,000 patients. Those with three or more major health conditions had a 40% higher risk of serious complications after anesthesia, regardless of how many times they’d had it before.
Individual sensitivity is real. Some people react badly to certain drugs. Maybe you felt nauseous for days after your first surgery. Or your heart rate dropped dangerously low during your second. Those aren’t "one-off" events. They’re signals. Your anesthesiologist will avoid those drugs next time. But if you keep needing surgery and your body keeps reacting poorly, options shrink. That’s when the real concern begins-not because you’ve had anesthesia too many times, but because your body is sending red flags.
What Happens If You’ve Had Too Many?
There’s no official "too many" threshold. But there are warning signs doctors watch for:
- Recovery takes longer than usual-hours instead of minutes.
- You need higher doses to get the same effect.
- You develop unexplained confusion or memory issues after surgery.
- Your blood pressure or oxygen levels drop harder than before.
When these happen, your care team doesn’t just say, "You’ve had five times-time to stop." They ask: "Why is this happening?"
Maybe your liver is struggling to process the drugs. Maybe your airway is narrowing due to scar tissue from past intubations. Maybe you’ve developed a rare condition called malignant hyperthermia, which can be triggered by repeated exposure to certain anesthetics. These aren’t common, but they’re real. And they require a full medical review before any future procedure.
How Do Doctors Decide If It’s Safe Again?
Every time you schedule surgery, you’ll meet with an anesthesiologist. They don’t just glance at your chart. They dig into:
- Previous anesthetic records-what drugs were used, how you reacted, how long you took to wake up.
- Your current medications, including supplements. Some herbs like ginkgo or garlic can interfere with blood clotting during surgery.
- Your lung and heart function. A simple EKG or breathing test can reveal hidden risks.
- Your weight and body composition. Obesity changes how drugs are absorbed and distributed.
If you’ve had five or more anesthetics in the last five years, they’ll likely order extra tests. A full cardiac workup. A sleep study if you snore. Blood tests to check liver enzymes. They’re not being cautious because you’ve had too many. They’re being cautious because your history tells them to look deeper.
Private Surgery and Anesthesia: Why Timing Matters
In private healthcare, you often have more control over when you schedule surgery. That’s a big advantage. Waiting too long for a procedure can make anesthesia riskier.
For example, if you’ve had chronic knee pain for three years and avoided surgery because you were afraid of anesthesia, your body might be in worse shape by the time you finally act. You might have gained weight. Your heart might be weaker. Your muscles might be atrophied. All of that increases anesthesia risk.
On the other hand, if you get surgery sooner-while you’re still active, healthy, and managing your weight-the procedure is safer, recovery is faster, and the chance of needing repeat surgeries drops.
That’s why many private clinics encourage early intervention. It’s not just about cost or convenience. It’s about reducing long-term anesthesia exposure by preventing complications that lead to more surgeries.
Alternatives to Repeated Anesthesia
Not every procedure needs general anesthesia. Ask your surgeon and anesthesiologist about alternatives:
- Regional blocks: Numbing just your arm, leg, or lower body. You stay awake. No breathing tube. Lower risk.
- Local anesthesia with sedation: A small injection plus mild IV sedation. Used for many dental, skin, and minor orthopedic procedures.
- Minimally invasive techniques: Keyhole surgery often needs less anesthesia than open surgery.
- Non-surgical options: Physical therapy, injections, nerve stimulation. Sometimes these delay or even eliminate the need for surgery.
One patient I worked with had three knee surgeries under general anesthesia over seven years. Each time, she had trouble waking up and felt foggy for days. After her third, her anesthesiologist suggested a spinal block for her next procedure. She had it. Woke up in 20 minutes. Walked out the same day. No nausea. No confusion. She’s now planning to avoid surgery altogether with a targeted rehab program.
What You Can Do to Stay Safe
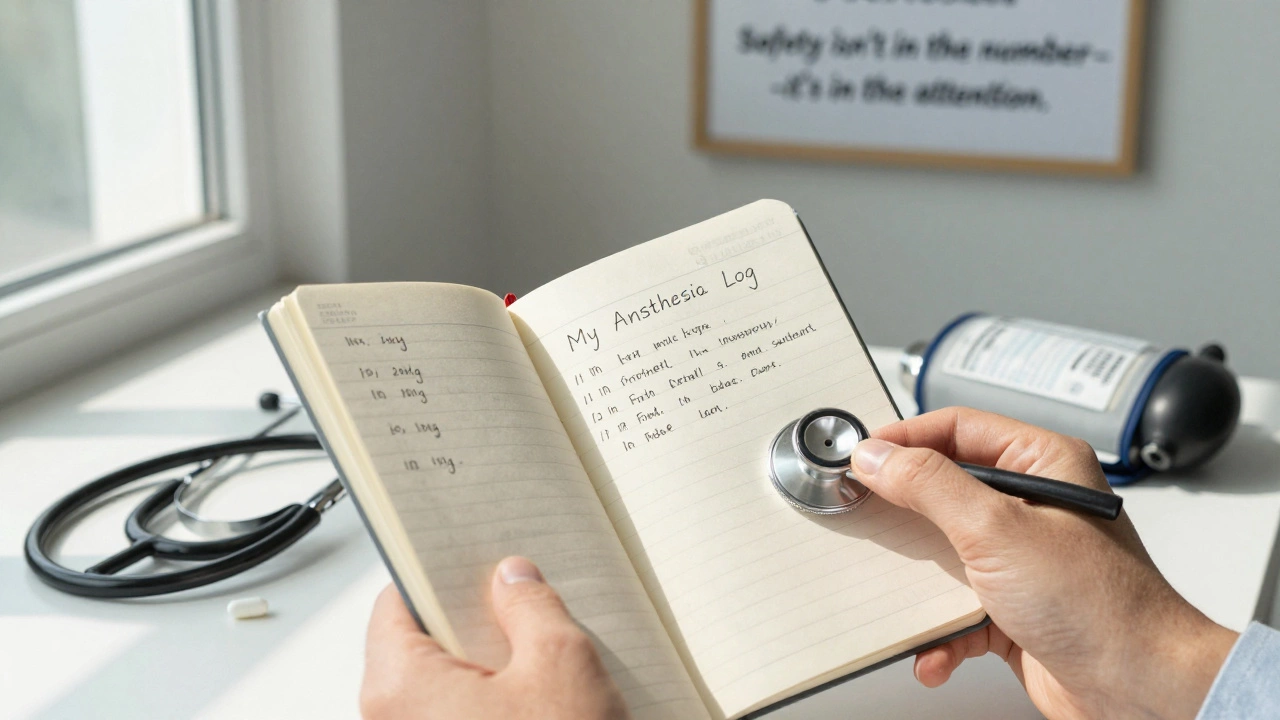
If you’ve had multiple anesthetics-or are planning more-here’s what actually helps:
- Keep a personal anesthesia log. Write down the date, surgery type, drugs used, how you felt afterward, and any side effects. Bring this to every pre-op appointment.
- Optimize your health before surgery. Lose weight if needed. Quit smoking. Control blood pressure and blood sugar. Even small improvements reduce risk.
- Ask about alternatives. Don’t assume general anesthesia is the only option. Push for a discussion.
- Choose experienced providers. Private hospitals with high-volume anesthesia teams have lower complication rates. Ask about their success rates.
- Follow recovery advice. Rest, hydrate, avoid alcohol. Poor recovery after one surgery can make the next one riskier.
Final Thought: Anesthesia Is a Tool, Not a Threat
Modern anesthesia is incredibly safe. For healthy people, the risk of death from anesthesia is lower than the risk of dying in a car crash on the way to the hospital. But safety isn’t guaranteed by frequency. It’s guaranteed by attention.
Every time you go under, your medical team should treat it like the first time-because your body changes. Your risks change. Your needs change.
If you’re considering another surgery, don’t ask, "How many times is too many?" Ask, "What’s the safest way to do this for me right now?"
Can anesthesia damage your brain over time?
For most healthy people, no. A single or even multiple exposures don’t cause brain damage. But in older adults-especially those over 65 with existing cognitive issues-there’s a small risk of temporary confusion or memory lapses after surgery, known as postoperative cognitive dysfunction. This usually clears up in weeks or months. Long-term damage is extremely rare and typically only seen in cases with severe complications like prolonged low oxygen.
Is it safer to have multiple surgeries at once instead of separately?
Sometimes, yes. Having two procedures under one anesthetic means one exposure instead of two. But only if it’s medically appropriate. Combining surgeries increases the overall surgical time and complexity, which can raise risks. Your team will weigh the benefit of fewer anesthetics against the risk of a longer, more complex operation. It’s not a one-size-fits-all call.
Do anesthetics build up in your body?
No. Modern anesthetic drugs are designed to be broken down and cleared quickly-usually within hours. They don’t accumulate like some painkillers or antidepressants. What matters isn’t leftover drug in your system. It’s how your body’s organs (liver, kidneys, lungs) are functioning at the time of the next surgery.
Can you become addicted to anesthesia?
No. Anesthesia drugs like propofol or sevoflurane aren’t addictive. They don’t trigger dopamine surges like opioids or alcohol. You won’t crave them. However, some people develop a fear of anesthesia after a bad experience, which is psychological-not physical addiction.
What if I’ve had anesthesia and now I’m pregnant?
Past anesthesia doesn’t affect pregnancy. There’s no evidence that previous exposure harms fertility or increases risks for your baby. But if you’re planning surgery while pregnant, your anesthesiologist will use different drugs and monitor you differently. Always tell them about your full anesthesia history-even if it was years ago.