Pain Tracker Calculator
Your Pain Log
Your Pain History
Summary for Your Doctor
If you’ve been living with chronic pain for months or years, you know it’s not just a number on a scale. It’s the sleep you lose, the plans you cancel, the way your body feels like it’s working against you every single day. And when your current pain meds aren’t doing enough, asking your doctor for more can feel impossible. You fear being labeled as a drug seeker. You worry they’ll shut you down. You’re not alone. Millions of people with chronic pain face this same moment - and most don’t know how to ask the right way.
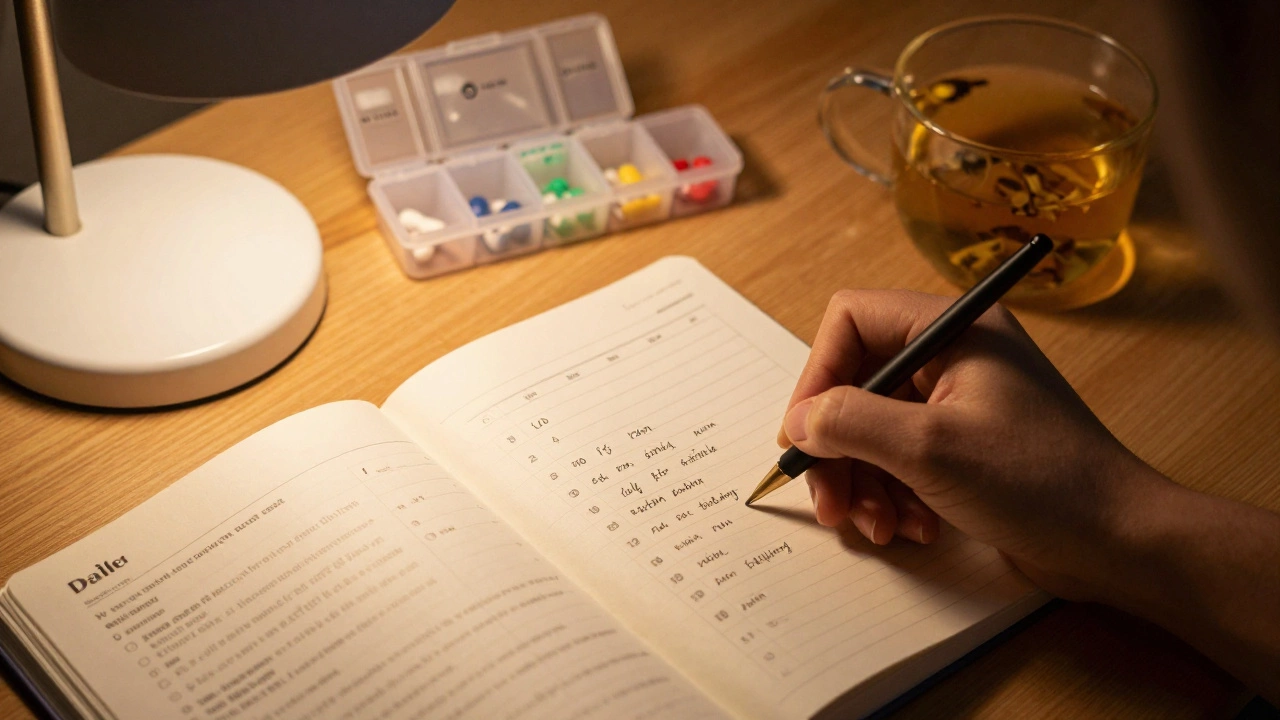
Start with facts, not feelings
Don’t say, “I’m in so much pain, I need more meds.” That’s a conversation stopper. Doctors hear that every day, and it triggers suspicion. Instead, come prepared with data. Track your pain for at least a week before your appointment. Use a simple notebook or a free app like PainScale or MyTherapy. Write down:- What time of day your pain peaks
- What makes it worse (walking, sitting, weather)
- What makes it better (heat, rest, meds)
- How much relief you get from your current dose
- How many hours the meds actually last
For example: “My current dose of 10mg oxycodone lasts 3 hours. I take it at 7 a.m., 11 a.m., and 4 p.m., but by 8 p.m., I’m doubled over. I can’t sleep, and I can’t sit through dinner with my family.” That’s specific. That’s measurable. That’s what your doctor needs to hear.
Bring your treatment history
Doctors don’t just look at your pain level - they look at your pattern. If you’ve tried everything else, say so. List what you’ve already done:- Physical therapy (how many sessions? Did it help?)
- Alternative treatments (acupuncture, TENS, massage)
- Over-the-counter meds (ibuprofen, acetaminophen - and how much you took)
- Other prescriptions you’ve tried and why you stopped
If you’ve had a nerve block, steroid injection, or surgery, mention it. If you’ve been to a pain specialist before, bring their notes. Showing you’ve exhausted other options tells your doctor you’re not looking for a quick fix. You’re looking for a solution.
Know your medication options
Not all pain meds are the same. If you’re on a short-acting opioid like hydrocodone and it’s wearing off too fast, you might need a long-acting one like extended-release oxycodone or a fentanyl patch. If you’re on gabapentin and it’s not touching your nerve pain, pregabalin might work better. If you’ve been on NSAIDs for years and your stomach is killing you, maybe a COX-2 inhibitor like celecoxib is safer.Don’t say, “I need more.” Say, “I’ve been on 10mg oxycodone three times a day for six months. My pain is still at 8/10. I’ve tried gabapentin and naproxen, but they didn’t help. I’ve read that long-acting options might help me stay steady through the night. Can we talk about switching?”
Doctors are more likely to respond to a thoughtful suggestion than a demand. You’re not arguing - you’re collaborating.
Ask about non-opioid options too
Even if you want more opioids, don’t only ask for them. Ask about other tools that might reduce your reliance on pills:- Can I get a referral to a pain psychologist? Studies show CBT reduces pain perception by 30-50% in chronic pain patients.
- Is there a local pain clinic that offers multidisciplinary care? Many combine meds with physical therapy, counseling, and nerve stimulation.
- Could I try topical lidocaine patches or capsaicin cream? They’re low-risk and help localized pain.
When you show you’re open to other approaches, your doctor sees you as someone who wants to get better - not someone who just wants pills. That builds trust.
Be ready for pushback - and how to handle it
Your doctor might say no. Or they might say, “We’re cutting back on opioids.” That’s not personal. It’s policy. In 2025, most clinics follow CDC guidelines that discourage long-term opioid use unless absolutely necessary. But that doesn’t mean you’re out of options.If they refuse:
- Ask: “What would it take for you to increase my dose?”
- Ask: “Can we try a short-term increase for 2 weeks while I start physical therapy?”
- Ask: “Can you refer me to a pain specialist?”
Many primary care doctors don’t feel comfortable managing high-dose opioids. A pain management specialist might be the next step. These doctors see 30-40 chronic pain patients a day. They know how to titrate doses safely and when to add non-opioid tools.
What not to do
Avoid these mistakes - they’ll hurt your case:- Don’t say, “My other doctor gave me more.” That sounds like you’re shopping.
- Don’t mention online pharmacies or buying meds on the street. Ever.
- Don’t exaggerate. “I can’t even breathe” when you’re sitting calmly in the chair? That undermines you.
- Don’t show up late, hungover, or high. You’ll lose credibility instantly.
Your goal isn’t to win an argument. It’s to be seen as a responsible, informed patient who deserves thoughtful care.
What if your doctor still says no?
If your doctor refuses to adjust your meds and you feel dismissed, you have options:- Request a copy of your medical record. Review it for accuracy. If your pain level is listed as “mild” when you’ve rated it “8,” correct it.
- Ask for a referral to a pain clinic. Many insurance plans cover them.
- Find a new doctor. Use the American Academy of Pain Medicine’s directory or ask your local hospital for recommendations.
- Consider a second opinion. You have the right to one.
Chronic pain is a medical condition, not a character flaw. You’re not weak for needing help. You’re not a addict for wanting relief. You’re someone who’s been fighting for years - and you deserve a doctor who listens.

What to bring to your appointment
Walk in prepared. Bring:- A pain log (even a screenshot from your phone app)
- A list of all current meds (including doses and times)
- A list of treatments you’ve tried
- Questions written down (don’t rely on memory)
- A friend or family member to help you remember what was said
Having someone with you can help. They can confirm your pain levels, remind you of symptoms you forgot, and help you remember the doctor’s advice.
It’s not about getting more pills - it’s about getting better
The goal isn’t to max out your prescription. The goal is to live. To sleep. To hold your grandchild. To walk to the mailbox without crying. Medication is one tool. Physical therapy, mental health support, nerve blocks, and lifestyle changes are others.When you walk into that office, you’re not begging. You’re advocating. You’ve done your homework. You’ve tracked your pain. You’ve tried other options. You’re ready to work with your doctor - not against them.
That’s how you get heard.
Can my doctor refuse to give me more pain meds even if I’m in real pain?
Yes, doctors can refuse - but not because your pain isn’t real. Many are bound by clinic policies, insurance rules, or fear of legal scrutiny. That doesn’t mean you’re out of options. Ask for a referral to a pain specialist, request a second opinion, or seek care at a dedicated pain clinic. These providers have more experience managing complex cases and are trained to balance safety with effectiveness.
How long does it take to get a higher dose of pain medication?
There’s no fixed timeline. Some doctors will adjust your dose within a week if you’ve shown consistent pain patterns and no red flags. Others require 30-60 days of documentation, urine tests, and follow-ups. If your pain is severe and uncontrolled, ask for a short-term increase (like 1-2 weeks) while you start other therapies. This shows you’re not asking for more indefinitely - you’re looking for a plan.
Are there legal limits on how much pain medication a doctor can prescribe?
In the U.S., there’s no federal cap on opioid prescriptions, but many states have laws limiting initial prescriptions to 7 days for acute pain and requiring regular monitoring for chronic use. Some insurers require prior authorization for doses over 90 MME (morphine milligram equivalents) per day. Your doctor must follow state and insurance rules - but they can still prescribe higher doses if they document medical necessity and follow safety protocols.
What if I can’t afford my current pain meds?
Ask your doctor about generic alternatives. For example, oxycodone ER (generic OxyContin) is often cheaper than brand-name versions. Many pharmaceutical companies offer patient assistance programs. You can also check NeedyMeds.org or GoodRx for discounts. Some clinics have sliding-scale fees or free medication samples. Don’t skip doses because of cost - talk to your doctor. They may have resources you don’t know about.
Can I switch doctors if mine won’t help me with pain meds?
Absolutely. You have the right to change providers. If your doctor consistently dismisses your pain, refuses to listen, or makes you feel judged, it’s time to find someone else. Look for a board-certified pain management specialist. Ask for recommendations from local support groups or hospitals. Your pain matters - and you deserve a doctor who treats it that way.
Next steps if you’re struggling
If you’ve tried everything and still feel unheard:- Join a chronic pain support group (online or in-person). You’ll learn what works for others.
- Keep your pain log going - even if your doctor doesn’t listen now, it’ll help if you switch providers.
- Consider seeing a pain psychologist. They don’t tell you to “think positive.” They teach you how to live better with pain.
- If you’re in crisis - thoughts of self-harm, feeling trapped - call the 988 Suicide & Crisis Lifeline. You’re not alone.
Chronic pain doesn’t go away overnight. But with the right approach, you can get relief - and the respect you deserve.




